What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
Who Is Vulnerable to Developing Gout?

Gout, often characterized by sudden and intense pain, swelling, and redness in the joints, primarily affects individuals who exhibit certain predisposing factors. Men over the age of 40 are particularly susceptible, as are postmenopausal women due to hormonal changes. Additionally, those with a family history of gout are at an increased risk, suggesting a genetic component to the condition. Lifestyle choices can also play a significant role. Excessive alcohol consumption, particularly beer, and a diet rich in purine-containing foods such as red meat, seafood, and organ meats can elevate the risk. Additionally, obesity and conditions like high blood pressure, diabetes, and kidney disease are associated with a higher likelihood of developing gout. Taking certain medications, such as diuretics, can contribute to elevated uric acid levels, increasing the likelihood of gout flare-ups. If you have had one or more gout attacks, it is strongly suggested that you are under the care of a podiatrist who can help you to manage this condition.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact David K. Morris, DPM from Florida. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions please feel free to contact our office located in Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Everything You Need to Know About Gout
Gout, typically found in diabetic patients, is an unusually painful form of arthritis caused by elevated levels of uric acid in the bloodstream. The condition typically strikes the big joint on the big toe. It has also been known to strike the knees, elbows, fingers, ankles and wrists—generally anywhere that has a functioning, moving joint.
The high level of uric acid in a person’s bloodstream creates the condition known as hyperuricema—the main cause of gout. Genetic predisposition occurs in nine out of ten sufferers. The children of parents who suffer gout will have a two in ten chance of developing the condition as well.
This form of arthritis, being particularly painful, is the leftover uric acid crystallizing in the blood stream. The crystallized uric acid then travels to the space between joints where they rub, causing friction when the patient moves. Symptoms include: pain, redness, swelling, and inflammation. Additional side effects may include fatigue and fever, although reports of these effects are very rare. Some patients have reported that pain may intensify when the temperature drops, such as when you sleep.
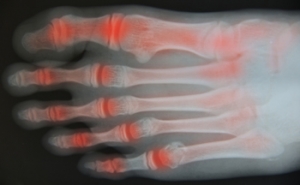
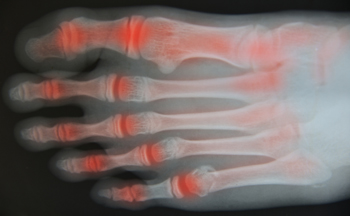
Most cases of gout are easily diagnosed by a podiatrist’s assessment of the various symptoms. Defined tests can also be performed. A blood test to detect elevated levels of uric acid is often used as well as an x-ray to diagnose visible and chronic gout.
Treatment for gout simply means eliminating symptoms. Non-steroid anti-inflammatory drugs or NSAIDs (Colchicine and other corticosteroid drugs, etc.) will quell the redness, the swelling, and the inflammation. However, managing your diet, lifestyle changes, and using preventative drugs are all helpful toward fully combating the most severe cases.
Those that lead an inactive lifestyle are at a higher risk for gout. Any amount of exercise decreases the probability of repeat encounters with the condition. Reducing your consumption of red meat, sea food, and fructose-sweetened drinks also reduces the likelihood of chronic gout as well.
Ingesting Vitamin C, coffee, and particular dairy products can help with maintaining a healthy lifestyle. There are new drugs out on the market that inhibit the body’s production of uric acid-producing enzymes. However, reducing or eliminating your overall levels of uric acid is the best remedy to ensuring you lead a gout-free life.
Exercise May Provide Relief for Arthritis
Arthritis, a condition characterized by inflammation and stiffness in the joints, can significantly impact one's quality of life. While medications and therapies are commonly prescribed to manage arthritis symptoms, the power of exercise in providing relief cannot be overstated. Regular physical activity helps to maintain joint flexibility, strengthen muscles surrounding the joints, and improve overall mobility. Low-impact exercises such as walking, swimming, and cycling are particularly beneficial for individuals with arthritis, as they minimize stress on the joints while promoting cardiovascular health and muscle strength. Additionally, exercises focusing on range of motion and flexibility, such as yoga and tai chi, can help alleviate stiffness and improve joint function. Engaging in consistent exercise routines not only reduces pain and inflammation but also enhances mood and promotes a sense of well-being. If you have arthritis and it is affecting your feet, it is suggested that you consult a podiatrist who can provide you with specific stretches and treatment targeted for relief.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact David K. Morris, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our office located in Plantation, FL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Arthritic Foot Care
During your lifetime, you will probably walk about 75,000 miles, which is quite a lot of stress to put on your feet. As you get older, the 26 bones and 30 joints in each of your feet will lose flexibility and elasticity. Your foot’s natural shock absorbers will wear down as well. Having arthritis added to this mix only makes matters worse. Your joints will become distorted and inflamed, which is why arthritic foot care needs to be something to think about every day.
When dealing with arthritis, having additional foot complications, such as bunions, hammertoes, or neuroma, can be a serious detriment. To avoid these, buy well-fitting shoes with a lower heel and good support. Arthritis causes you to lose your arch, so having shoes with good arch support is also highly recommended.
Aside from getting good arch support, the shoes need to fit comfortably and properly as well. A good place to start is by leaving a finger width between the back of the shoe and your foot to gauge proper size. It is also helpful to have a square or rounded toe box in the front to provide even more comfort. Another thing to look for is a rubber sole that can provide a cushion and absorb shock as you walk. This adds flexibility to the ball of your foot when you push off your heel to walk.
Exercise is another key aspect of arthritic foot care. Exercise not only strengthens and stretches your muscles and joints, but helps to prevent further injury and pain as well. Stretching the Achilles tendon, the tendon located in the back of your heel, will give you added mobility and reduce pain due to stress. Another thing you can do is massage your feet, kneading the ball of your foot as well as your toes from top to bottom.
Stretching the Achilles tendon is a simple exercise that you can do at home anytime. Lean against the wall with your palms flat against the surface while placing one foot forward, towards the wall, and one foot behind you. Bend your forward knee towards the wall while keeping your back knee locked straight, and make sure both your heels are completely touching the ground at all times. This will stretch your Achilles tendon and calf muscles as well. You will feel the stretch almost immediately. You can also stretch your toes in a couple ways. One involves taking a rubber band and wrapping it around both your big toes while your heels remain together. Then, pull them apart to stretch your big toe. You can also place a rubber band around all the toes of one of your feet. Then, try to separate each individual toe, stretching them all.
A final step you can take to help your arthritis is taking non-steroid, non-inflammatory drugs or topical medicines with capsaicin. Unfortunately, there is no complete way to remove all of your arthritic pain. However, following some of this advice can go a long way in staying as pain-free as possible.
Signs and Symptoms of Foot Neuropathy

Foot neuropathy, a common complication of various medical conditions such as diabetes, refers to nerve damage that affects sensation and function in the feet. One of the primary indicators of foot neuropathy is tingling or burning sensations in the feet, often accompanied by numbness or loss of feeling. This diminished sensation increases the risk of injury and can lead to unnoticed wounds or ulcers. Additionally, individuals with foot neuropathy may experience sharp or shooting pains, especially during movement or when pressure is applied to the affected areas. Muscle weakness and difficulty coordinating movements are also common symptoms, making it challenging to walk or perform routine tasks. Recognizing these signs early is essential for timely intervention and management to prevent complications. If you have any of the above symptoms, it is suggested that you are under the care of a podiatrist who can offer you relief and management tips.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with David K. Morris, DPM from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is the weakness, numbness, and pain in the hands and feet due to damage to the peripheral nerves. The peripheral nerves are responsible for sending information from the brain and spinal cord to the rest of your body. Causes of Neuropathy include: traumatic injuries, infections, metabolic problems, exposure to toxins, and diabetes.
Diabetes is the most common cause, with more than half of the diabetic population developing some type of neuropathy. There are several types of neuropathy and they vary based on the damage of the nerves. Mononeuropathy is classified as only one nerve being damaged. When multiple nerves are affected, it is referred as polyneuropathy. One of the types of polyneuropathy is distal symmetric polyneuropathy. It is the most common for people with diabetes and starts when the nerves furthest away from the central nervous begin to malfunction. The symptoms begin with pain and numbness in the feet and then they travel up to the legs. A rarer form of polyneuropathy is acute symmetrical peripheral neuropathy, which is a severe type that affects nerves throughout the body and is highly associated with Guillain-Barre syndrome, an autoimmune disorder that attacks the peripheral nervous system and can be fatal. Although there are many types of neuropathy, most of them share the same symptoms such as pain, extreme sensitivity to touch, lack of coordination, muscle weakness, dizziness, and digestive problems. Since neuropathy affects the nerves, those affected should be careful of burns, infection and falling, as depleted sensations disguise such ailments.
The best way to prevent neuropathy is to manage any medical conditions such as diabetes, alcoholism, or rheumatoid arthritis. Creating and managing a healthy lifestyle can also go a long way. Having a healthy diet full of fruits, vegetables, whole grains and lean protein can keep the nerves healthy. These types of food have the nutrients to prevent neuropathy. Regularly exercising can help as well, but it is best to consult with a doctor about the right amount. In addition to diet and exercise, avoiding risk factors will also prevent neuropathy. This includes repetitive motions, cramped positions, exposure to toxic chemicals, smoking and overindulging on alcohol.
Are Bunions Affecting Your Everyday Life?
Recovering From Ankle Replacement Surgery

Total ankle replacement, also known as total ankle arthroplasty, is a significant surgery aimed at relieving ankle pain. During the procedure, the surgeon removes parts of the shin bone, or tibia, and the top portion of the foot's highest bone, the talus, replacing the ankle with plastic or metal components. After surgery, you will likely have a cast, boot, or splint on your leg for approximately a month, and you will not be able to put weight on it immediately. You may need crutches, a walker, or a knee scooter during this time. It is important to have assistance at home during the initial recovery period. You will be discharged with bandages and stitches or staples, which your doctor will advise you on when to remove. Post-surgery, you may experience mild pain and swelling, for which your doctor may prescribe medication. Rehabilitation exercises, which are important for regaining strength and mobility, will continue for several weeks. Returning to work depends on individual recovery speed and job requirements, with certain movements or weight-bearing activities possibly restricted. If you have had your ankle replaced, it is suggested that you are under the care of a podiatrist who will provide personalized recovery steps for the most successful outcome.
In certain cases, in which the patient suffers from extreme pain or damage in a joint, joint replacement surgery may be deemed useful. If you have constant pain in a foot joint, consult with David K. Morris, DPM from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Joint Replacement Surgery?
Over time, joints wear down; this can be exacerbated by diseases and conditions. Joint replacement surgery, also known as arthroplasty, is when a damaged joint is surgically removed and replaced with a prosthesis. Prostheses, which can be made of ceramic, plastic, or metal, act as joints in lieu of an actual joint. One of the most prevalent causes for joint replacement is arthritis.
Arthritis in the Foot
Arthritis can occur in any joint in the body, including in the feet. Common types of arthritis in the foot are osteoarthritis, rheumatoid arthritis, and gout. The big toe is usually where arthritis occurs in the foot; this is known as hallux rigidus.
Joint Replacement Surgery in the Foot
The most common form of joint replacement in the foot is a first metatarsophalangeal (MTP) joint placement. MTP joint replacement surgery is designed to treat hallux rigidus. Surgery is not intensive, and recovery occurs within one to two months after the procedure has been done. Overall, joint replacement surgery is a safe and effective way to treat pain in the joint of the foot.
If you have any questions, please feel free to contact our office located in Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Joint Replacement Surgery
When conservative, noninvasive treatments prove unsuccessful, podiatrists will often turn to surgery as the last line of treatment for their patients. If patients are suffering from joint pain, issues in mobility, or are seeking to correct a deformity, joint replacement surgery is an effective option. Joint replacement surgery is also successful in treating arthritis, which is the most common cause of improperly working joints.
Patients with symptoms that include joint pain, stiffness, limping, muscle weakness, limited motion, and swelling are typically considered for joint replacement surgery. Range of motion and activity post-surgery will vary between patients and depending on the specific surgery performed, the affected joint, and the damage that will need to be repaired.
Joint replacement surgery replaces the damaged cartilage and bone, the latter if required. The damaged cartilage is typically replaced with a prosthesis that is attached to the bone, allowing the implant to grow into the bone. Following surgery, the patient will typically undergo physical therapy to become familiar with movement using the replaced joint.