The Hidden Dangers of Flip-Flops on Your Feet
 Flip-flops, though convenient, can be harsh on your feet, especially for individuals at risk like those with diabetes. The lack of support in flip-flops leads to improper heel strike, causing stress on the heels and increasing the risk of plantar fasciitis. Further, to keep the flip flops on, wearers often grip with their toes, which can cause muscle strain and negatively affect conditions like hammertoes. For people with diabetes, the minimal protection provided by flip-flops increases the risk of cuts, blisters, and infections due to decreased sensation and poor wound healing. Additionally, the flat design offers little or no arch support, leading to pain and discomfort in the feet and ankles. If you have foot pain as a result of wearing flip-flops, it is suggested that you consult a podiatrist who can offer you relief tips, in addition to guiding you on more favorable footwear choices.
Flip-flops, though convenient, can be harsh on your feet, especially for individuals at risk like those with diabetes. The lack of support in flip-flops leads to improper heel strike, causing stress on the heels and increasing the risk of plantar fasciitis. Further, to keep the flip flops on, wearers often grip with their toes, which can cause muscle strain and negatively affect conditions like hammertoes. For people with diabetes, the minimal protection provided by flip-flops increases the risk of cuts, blisters, and infections due to decreased sensation and poor wound healing. Additionally, the flat design offers little or no arch support, leading to pain and discomfort in the feet and ankles. If you have foot pain as a result of wearing flip-flops, it is suggested that you consult a podiatrist who can offer you relief tips, in addition to guiding you on more favorable footwear choices.
Flip-flops are not always the best choice of footwear. If you have any concerns about your feet or ankles, contact David K. Morris, DPM from Florida. Our doctor will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
When the weather starts warming up, people enjoy wearing flip-flops. Flip-flops are comfortable, stylish, and easy to slip on and off; they're perfect for any summer beach goer. However, these shoes can cause harm to the feet.
How Can Flip-Flops Affect Me Long-Term?
- Ankle problems
- Hip problems
- Lower back problems
- Pain in the balls of the feet
- Problems with foot arches
- Changes in the way you walk
Are There Injuries Associated with Flip-Flops?
Yes. Since flip-flops are relatively weak and do not provide the same amount of support as sneakers, people who wear flip-flops regularly are more susceptible to injuries. On top of that, the open nature of the shoe makes your feet more prone to other problems, such as cuts and even infections. Common injuries and ailments include:
- Sprained ankles
- Blisters
- Infections
- Cuts and Scrapes
I like Wearing Flip-Flops. Are There Safe Alternatives?
When buying flip-flops, try to find ones that have sturdy soles and that are made of high-quality materials that will support for your feet. These flip-flops will cost more but will also last longer as a result.
If you have any questions please feel free to contact our office located in Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flip Flops and Feet
Flip flops are often a popular choice of footwear for many people. Flip flops allow your feet to breathe and give your toes the freedom of movement. They are easy to slip on and can be worn with virtually any style of clothing. Flip flops, however, despite their many benefits, can be detrimental for your foot health.
Despite their comfortableness, frequently wearing flip flops can create problems in the lower body over time. Issues mainly stem from the fact that people walk differently in flip flops compared to other footwear, such as sneakers. This is due to a change in one’s natural gait, which therefore creates stress in different parts of the body while hindering the body’s natural posture. Problems can also arise in the arches and balls of the feet. Flip flops provide little to no support to these areas.
Aside from long-term problems, flip-fops can also create short-term issues as well, such as ankle sprains and blisters. Weak materials that are flexible and bendable are generally used to manufacture flip flops. These materials make its wearers prone to both tripping and injuring their ankles. Flip flops can create blisters as the material rubs against the foot. People are much more at risk for infection while wearing flip flops due to their openness. This also makes it easier to scrape and cut the foot since there is a lack of protection. If these cuts are left untreated and uncovered, the risk then becomes greater.
To prevent the aforementioned occurrences, purchase a pair of flip flops that offer significant protection. The soles of the flip flops should not be floppy, but sturdy and firm, and should not significantly bend or wiggle when lifted from the floor. Flip flops made of high-quality materials will not be affected by this problem. While higher quality flip flops may be more expensive, they will last longer and provide better protection compared to a cheaper pair. Brand name flip flops sold from a quality manufacturer are a dependable option.
There is no problem in wearing your favorite pair of flip flops so as long as you do not wear them daily or for extended periods of time. Flip flops should be replaced every 3-4 months to ensure that they provide your feet with the best protection.
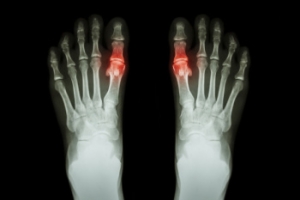
Understanding Pediatric Gout
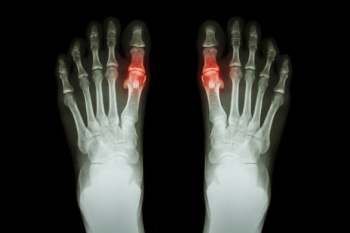
Pediatric gout, although rare, is a form of arthritis that affects children and is characterized by the accumulation of uric acid crystals in the joints. This condition can cause sudden and severe pain, swelling, redness, and warmth in the affected joints, most commonly the big toe. Symptoms may also include fever and limited joint movement due to intense discomfort. Risk factors for pediatric gout include genetic predisposition, obesity, and certain medications. Medical conditions that affect uric acid metabolism, such as leukemia or kidney disease, are other risk factors. Early diagnosis is essential for effective management, which typically involves medication to reduce uric acid levels and inflammation, along with lifestyle modifications like a balanced diet and maintaining a healthy weight. If your child has periodic, but intense, toe or foot pain, it is strongly suggested that you consult a podiatrist who can accurately diagnose, treat, and manage gout.
Gout is a painful condition that can be treated. If you are seeking treatment, contact David K. Morris, DPM from Florida. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our office located in Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Gout
Gout is a form of arthritis that is caused by a buildup of uric acid crystals in the joints. This considered to be one of the most frequently recorded medical illnesses throughout history. Gout occurrences in the US have risen within the past twenty years and the condition now affects 8.3 million people which is 4% of all Americans. Researchers have found that gout affects men more than women and African-American men more than white men.
Symptoms of gout are warmth, swelling, discoloration, and tenderness in the affected joint area. The small joint on the big toe is the most common place for a gout attack to occur.
People who are obese, gain weight excessively, drink alcohol heavily, have high blood pressure, or have abnormal kidney function are more likely to develop gout. Furthermore, certain drugs and diseases are likely to increase levels of uric acid in the joints which eventually leads to gout. You are also more likely to develop gout if you eat a lot of meat and fish.
Many who experience gout attacks will experience repeated attacks over the years. Some people who have gout symptoms, may never have them again, but others may experience them several times a year. If you have gout symptoms throughout the year, you may have recurrent gout. Those who have gout should also be careful about their urate crystals collecting in their urinary tract, because this may lead to kidney stones.
Diagnosis for gout is done by checking the level of uric acid in the joints and blood. Your podiatrist may also prescribe medicine to reduce uric acid buildup in the blood, which will help prevent any gout attacks.
To treat gout, your podiatrist may also prescribe you Anti-inflammatory medication (NSAIDs) which will relieve the pain and swelling of a gout episode and it can also shorten a gout attack. Maintaining a healthy diet is also a proven method to prevent gout attacks.
Arthritis Can Cause Pain in the Feet and Ankles
Relief for Acute Ankle Sprains

Acute ankle sprains are often caused by sudden twists that stretch or tear ligaments surrounding the ankle, causing pain, swelling, and difficulty while walking. Immediate treatment for an acute ankle sprain is important for effective recovery and to prevent long-term complications. Supportive measures include a lace-up brace, an air stirrup brace, or an elastic compression wrap to stabilize the injured ankle and promote faster healing. Early mobilization, as tolerated by pain levels, has been shown to aid in quicker recovery and reduce the risk of chronic ankle instability. Pain relief medications can help to manage inflammation and discomfort. Athletes and those prone to recurrent sprains may wish to consider using ankle supports during sports to prevent future injuries. If you have recently sprained your ankle or are experiencing persistent discomfort, it is suggested that you schedule an appointment with a podiatrist for a personalized treatment plan to ensure proper healing, and to minimize the chance of future ankle problems.
Ankle sprains are common but need immediate attention. If you need your feet checked, contact David K. Morris, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains take place when the ligaments in your ankle are torn or stretched beyond their limits. There are multiple ways that the ankle can become injured, including twisting or rolling over onto your ankle, putting undue stress on it, or causing trauma to the ankle itself.
What Are the Symptoms?
- Mild to moderate bruising
- Limited mobility
- Swelling
- Discoloration of the skin (depending on severity)
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
Treatment of a sprain depends on the severity. Many times, people are told to rest and remain off their feet completely, while others are given an air cast. If the sprain is very severe, surgery may be required.
If you have suffered an ankle sprain previously, you may want to consider additional support such as a brace and regular exercises to strengthen the ankle.
If you have any questions please feel free to contact our office located in Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Three Grades of Ankle Sprains
An ankle sprain occurs when one or more ankle ligament gets overly stretched. Ligaments are strong bands of tissue that bind and support the bones and other structures that make up the ankle. In more severe ankle sprains, the ligament(s) tear—either partially or completely—and there may be an audible popping noise at the moment of injury.
Ankle sprains are quite common and can occur when the ankle rolls outwardly (eversion) or inwardly (inversion), causing the ligament(s) to stretch beyond normal limits, or even tear. Falls, twists, or blows to the ankle during sports or other activities can cause this injury, as well as wearing improper footwear, running on uneven surfaces, or having weak ankles.
Depending on the injury’s severity, an ankle sprain will be classified as Grade I, Grade II, or Grade III. Grade I sprains involve ligament(s) being overly stretched but not torn, with symptoms of mild pain, swelling, and ankle instability. There may also be some difficulty bearing weight. A Grade II sprain usually involves a partial tear of the ligament which brings more intensity in these symptoms, along with possible bruising. With a Grade III sprain, the ligament is completely torn, the symptoms are severe, and it may not be possible to put weight on the affected foot at all.
To diagnose and grade an ankle sprain, a podiatrist will perform a physical examination, checking for tenderness and range of motion in the ankle. For more severe sprains, X-rays or other imaging studies may be necessary.
It is vitally important to have an ankle sprain treated properly as improper healing often leads to future ankle sprains and possibly even chronic ankle stability. Treatment for an ankle sprain will vary, depending on its severity, and may include the RICE method (Rest/Ice/Compression/Elevation), physical therapy, bracing, medications, and possibly even surgery to repair a torn ligament. Rehabilitation is very important for the sprain to heal properly and to restore functionality.
Wearing the Right Shoes While Landscaping

Wearing the right shoes while landscaping is essential for both safety and comfort. Proper footwear provides the necessary support and protection for your feet during strenuous outdoor activities. Landscaping often involves uneven terrain, sharp tools, and heavy lifting, making sturdy shoes with good traction vital to prevent slips and falls. Shoes with reinforced toes and durable materials protect against injuries from tools or debris. Additionally, supportive shoes help reduce fatigue and prevent foot and ankle strain, enabling you to work longer and more efficiently. Good arch support and cushioning also contribute to overall foot health, reducing the risk of chronic conditions like plantar fasciitis. Investing in high-quality, appropriate footwear ensures that you can tackle landscaping tasks safely and comfortably. If you have injured your foot from wearing the wrong shoes while landscaping, it is suggested that you speak to a podiatrist who can treat the condition and discuss what type of shoes are needed while landscaping.
While working on the feet, it is important to take the proper care of them. For more information about working on your feet, contact David K. Morris, DPM from Florida. Our doctor will treat your foot and ankle needs.
Working on Your Feet
Standing on your feet for long periods of time can cause stress and pain in your feet. Your whole body may experience change in terms of posture, back pain, bunions, callouses and or plantar warts. There are ways to avoid these conditions with proper foot care, smart choices and correct posture.
Positive Changes
Negative heeled shoe – Choosing this shoe type places the heel slightly lower than the ball of the foot. These are great for overall foot health. Find shoes that fit you correctly.
Go barefoot – Our feet were not designed to be enclosed for all hours of the day. Try to periodically expose your feet to air.
Eliminate Pain
Foot Exercises – Performing simple exercises, incorporating yoga and doing stretches are beneficial. This will allow increased blood flow to the area and muscles of the foot.
Achilles tendon – Stretching the foot out flat on the floor will relax the calf muscles and tendon. These exercises can be performed almost anywhere. Make sure you add these exercises to your daily regimen.
With a little bit of this information and knowing more about foot health, you will notice changes. Foot stretches and proper footwear will help with pain and prevent further issues.
If you have any questions please feel free to contact our office located in Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Handle a Long Work Day on Your Feet
In 2014, the American Podiatric Medical Association surveyed 1,000 American adults and found that half of all respondents lived with foot pain. Fortunately, there are ways to avoid foot problems such as following a daily footcare routine and wearing proper footwear at work.
If you have a job that requires you to be on your feet, it is best that you do not wear flat sole shoes. Your heel should be slightly elevated (less than 2 inches, but at least ¼-inch) if you are going to be standing for a prolonged period. You should also make sure that the shoes you wear are not too small. Tight shoes may cut off circulation to your feet, which will result in pain and blisters. It is always best to purchase fitted shoes later in the day, because the feet tend to swell as the day progresses. It may also be helpful to buy shoes a half size larger if you plan on wearing custom orthotics or arch supports.
Your muscles may become stiff when you are constantly standing up. It is important to take breaks every hour to stretch and relax. One tip is to perform calf raises, because this exercise will help improve your circulation. To perform this stretch, you first need to stand on the edge of a step with your abdominal muscles pulled inward. You then need to grip the step with the balls of your feet with your heels hanging over the edge. Next, try to raise your heels above the step by a few inches while standing on your tiptoes; hold this pose for a second. You should then lower your heels back even to the platform. These calf raises should be done ten times for full effectiveness.
You should also take care of your feet while you are at home. One of the best ways to prepare your feet for a long day of work is to soak them in ice water. Doing so for 20 minutes will help fight the swelling and inflammation that results from being on your feet at work.
Nevertheless, if you are experiencing pain in your feet, you should seek help from your podiatrist. Your doctor will help treat any ailments you may have in addition to helping you prevent any other ailments from developing in the future.
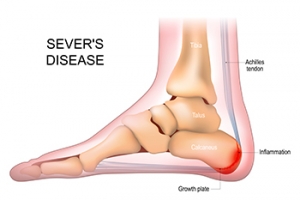
Causes and Impact of Sever’s Disease
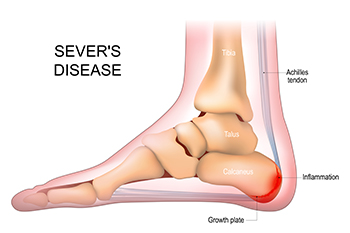
Sever's disease affects children and adolescents, particularly those engaged in physical activities like sports. It is not a disease but rather a disorder caused by inflammation of the growth plate in the heel bone, known as the calcaneal apophysis. This inflammation results from repetitive stress or tension on the heel bone, often during periods of rapid growth and development. Sever's disease typically affects children between the ages of eight and 14, when the growth plate is still open and vulnerable to injury. Activities that involve running, jumping, or high-impact movements can lead to heel pain, swelling, and tenderness, especially during or after physical activity. Sever's disease is not usually serious and typically resolves with rest and conservative treatments like stretching and heel cushions. However, it can temporarily limit a child's participation in sports and other activities, emphasizing the importance of proper management and injury prevention strategies. If your active child is complaining of heel pain, it is suggested that you schedule an appointment with a podiatrist who can properly diagnose and treat Sever’s disease.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see David K. Morris, DPM from Florida. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our office located in Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.